The paper “Perioperative Risk Prediction in Major Gynaecological Oncology Surgery: A National Diagnostic Survey of UK Clinical Practice“, co-authored by Lusine Sevinyan (University of Brighton), Anil Taylor (Department of Gynaecological Oncology, Royal Surrey NHS Trust), Pradeep Prabhu (Department of Anaesthetics, Royal Surrey NHS Trust), Peter Williams (Maths, Surrey), Melanie Flint (University of Brighton), and Thumuluru Kavitha Madhuri (University of Massachusetts & Royal Surrey NHS Trust), has been published in the MPDI Journal Diagnostics. The paper is published open access (link here).
The survey, which underpins the paper, explored how UK gynaecological oncology specialists used on-line websites to show patients the various medical issues that may arise during and after surgery. For instance, whilst open surgery enables better access to address internal problems, laparoscopic surgery leaves a much smaller scar and recovery time and is quicker (especially in terms of days in hospital). From a theoretical perspective, game theory comes to the fore, with a trade-off between potentially better long-term survival and poorer short-term quality of life. Underpinning the risk predictions, a battery of regression models are dynamically updated as data continue to be gathered.
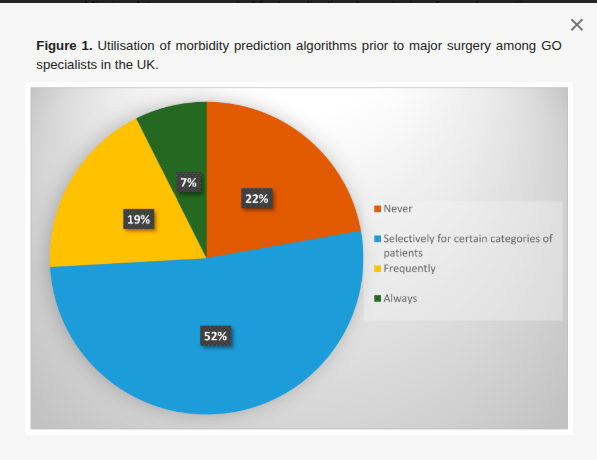
The results revealed considerable variation between specialists in terms of non-usage or usage of such websites, with respondents (all involved in surgical procedures) favouring different websites but expressing concern over the accuracy of various risk predictions (typically relating to complications after surgery).
A need was identified to adopt a definitive tool relating to risk prediction in gynaecological cancer operations. The most promising basis for this appears to be the website of the American College of Surgeons (ACS-NSQIP), which integrates unique procedural and patient-specific variables to deliver predictions for numerous postoperative complications and for length of hospital stay. Recommendations include prospective validation studies and tool integration into clinical workflows. Such diagnostics are positioned as essential to advancing precision surgery in gynaecological oncology by improving risk stratification, patient counselling, and institutional benchmarking. The image below shows Figure 1 from the paper (click on them to enlarge).